
1型糖尿病:iPS細胞での治験手術に成功
・糖尿病患者の経過は良好で、無事退院した
・術後は5年間経過を観察し、安全性を検証へ
読売新聞掲載記事からSummaryをお届けします。
京都大の矢部大介教授:京都市左京区:
4月14日、日本初となる1例目の治療を行ったと発表した。
1.iPS細胞を使い、重い1型糖尿病を治療する手術を実施した。
2.患者の経過は良好で、既に退院したという。
1型糖尿病とは:
1.1型糖尿病は10~15歳の発症が目立ち、患者は日本国内に推定10万~14万人。
2.通常、毎日数回のインスリン注射が必要だ。
重篤な患者が血糖値をうまくコントロールできなければ、低血糖になって意識を失い、死亡する危険性もある。
今回のiPS細胞での治験手術:
治験の対象は20~64歳の重篤な患者3人。
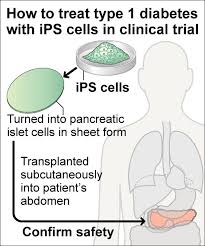
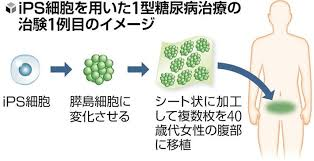
1.健康な人のiPS細胞から、 膵臓でインスリンを放出している膵島すいとう細胞を作製する。
2.数センチ四方のシートに加工し、患者の下腹部に複数枚を移植する。
術後は5年間経過を観察し、安全性や効果を検証する。

1例目の手術:
今年2月、京大病院で、40歳代女性にips細胞を移植した。
1.移植細胞から、インスリンが出ていることが確認された。
2.細胞が異常増殖するなど、安全性の問題はないとのこと。
3.女性は退院後も、自己注射を続けている。
京大病院は、移植細胞の生着とインスリンの分泌状況を確認する。
次回のiPS細胞手術内容:
1.次回2、3例目の手術で、移植する細胞数を段階的に増やす予定。
2.来年、2、3例の安全性に関する中間発表を行う。
その後、「シートを製造する京大の新興企業」が、欧米で国際共同治験を実施する。
矢部教授は今回の治療法について「2030年以降の実用化を目指す」と話した。
1型糖尿病の患者数:
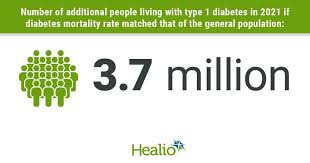
1.1型糖尿病の患者は、世界に推計800万人いる。
2.糖尿病のうち、1型は5%で、生活習慣の影響が大きい2型とは異なる。
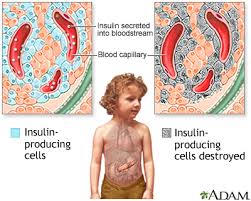
1型は、膵臓にある膵島細胞が、自己の免疫細胞などに破壊される。
また、血糖値を下げるインスリンが、ほとんど分泌されなくなる。
iPS細胞が糖尿病治療に貢献:
1型糖尿病の患者の悩み:
1.毎日のインスリン注射に耐えながら、暮らしている子どもの患者も多い。
2.新たな治療法で注射が不要になれば命を脅かす低血糖を回避できる。
2型糖尿病の患者の悩み:
現在、亡くなった人の膵島を移植しているが、ドナーが少ない。
1.将来的には中高年に多い2型糖尿病の重い患者も対象になる。
2.予備軍を含めて2型の患者は、日本に1000万人いる。

今後の課題:iPS細胞の大量生産
1.今回移植したiPS細胞数は、数千万個以上とみられる。
2.iPS細胞を使った他の病気の治療と比べてかなり多い。
1例目の患者は移植後まだ約2か月で、長期間の慎重な経過観察が必要だ。
「オリヅルセラピューティクス」(神奈川県):
「オリヅルセラピューティクス」がシートの製造を担当、iPS細胞を使った再生医療に取り組む。
京大と武田薬品工業が共同研究してきた技術を、同社が引き継いでいる。
https://www.yomiuri.co.jp/science/20250414-OYT1T50145/2/